The proposed work will provide a foundation for training navigators in digital health literacy which will support the growing needs for patients to engage with technology. This will ultimately be used to minimize disparities associated with unequal access to technology that have the potential to improve health outcomes.
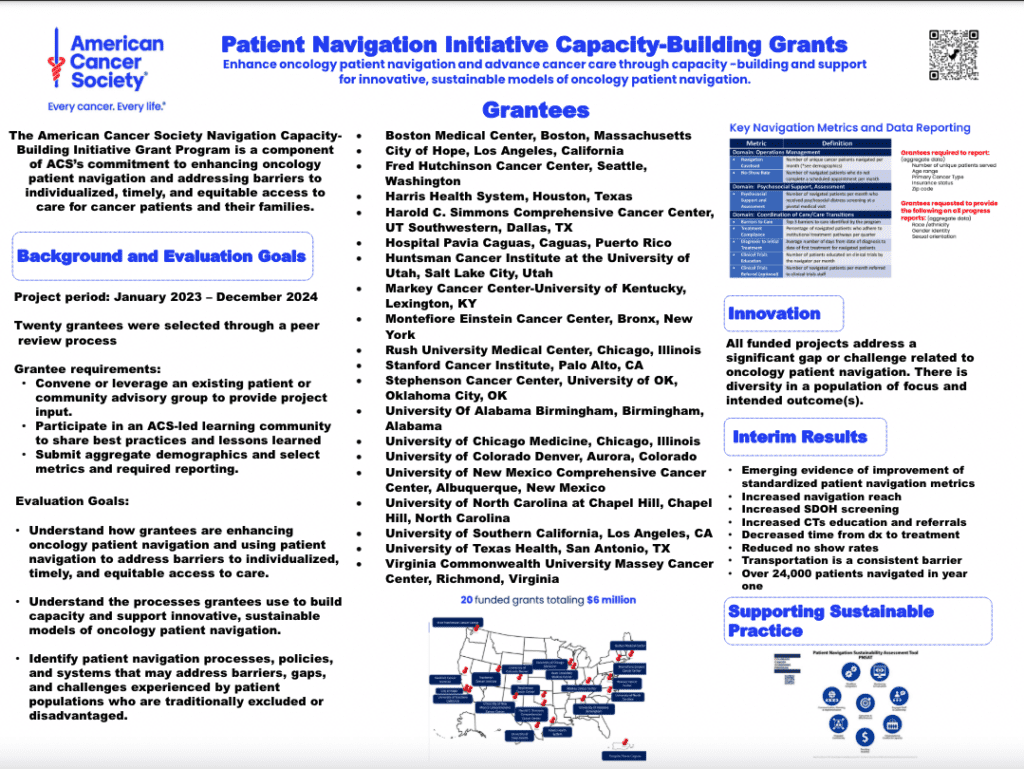
Navigators are lay and clinical individuals within the hospital system responsible for enhancing care coordination and proactively managing patient concerns.1 The navigation programs at the University of Alabama at Birmingham (UAB) and the University of South Alabama Mitchell Cancer Institute (MCI) emphasize support for vulnerable populations, including racial and ethnic minority groups (25%), rural residents (30%), and people who are socially disadvantaged (10% eligible for Medicare and Medicaid). In addition to supporting patients with barriers to healthcare delivery, the patient navigation workforce is ideally positioned to facilitate patient engagement with technology. Currently, at UAB and MCI, lay and nurse navigators use an electronic medical record integrated, web-based software (i.e. digital health tool) to capture patient-reported data, including symptoms, during both clinical encounters and at home. Our preliminary data shows that Black or African American (henceforth referred to as Black) patients were less likely to be enrolled (80% vs. 91%) and more likely to withdraw (20% vs. 9%) than White patients. In addition, patients living in rural areas had lower compliance rates (i.e. survey completion; 55% vs. 69%) when compared to patients living in urban areas. Our navigation teams expressed concerns regarding lack of training to specifically address barriers faced by patients with low digital health literacy. This proposal will include community-academic collaborations to address this need by meeting the following objectives: • Objective 1: Develop a basic training module for staff (navigators, social workers, nurses) on digital health literacy. This will include definitions, how to identify patients with low digital health literacy, and strategies to support patients with low digital health literacy. • Objective 2: Develop a hands-on training for lay navigators engaging patients in collection of patients reported outcomes that addresses digital health literacy. • Objective 3: Testing impact of training program in health systems where patient-reported outcomes are deployed as part of standard of care. • Objective 4: Disseminate training program to local, state, and national partners to use within their institutions. The proposed work will provide a foundation for training navigators in digital health literacy which will support the growing needs for patients to engage with technology. This will ultimately be used to minimize disparities associated with unequal access to technology that have the potential to improve health outcomes. BACKGROUND: The University of Alabama at Birmingham (UAB) and the University of South Alabama Mitchell Cancer Institute (MCI) has a long history of navigating patients with cancer. UAB has been a leader in the field of navigation, with continuous navigation services being provided for over 25 years. Dr. Rocque (PI) was the Medical Director for a Center for Medicare and Medicaid Innovation award, which implemented a lay navigation program across 12 cancer centers in the Southeastern US, including UAB and MCI.2 Over a 3-year period, this program employed lay navigators who provided an extra layer of support to more than 10,000 patients with cancer. 1 Navigators used routine distress screening during and between clinic visits via telephone to identify barriers to care and empower patients in overcoming these barriers.3 Navigators addressed 92% of patient concerns, and 90% of patients stated they would recommend the program to others.1 When compared with matched, non-navigated control patients, ED visits, hospitalizations, and ICU admissions for navigated patients declined by 6%, 8%, and 11% more per quarter, respectively. Reduced utilization led to reduced costs. For navigated patients, cost also declined by $780 more per quarter per patient compared to control patients.4 Navigators are a natural workforce for effective implementation of technology solutions to support patients during their cancer journey. Navigators are lay and clinical individuals within the hospital system responsible for enhancing care coordination and proactively managing patient concerns. 1 Patient navigation programs have proven efficacious for increasing access to care, care coordination, symptom management, and reducing cost.5-11 Provision of navigation services is mandated for certification by the Commission on Cancer,12 required for participation in Medicare’s payment reform demonstration project involving ~25% of US cancer patients (the Oncology Care Model),13 and advocated for by the National Academy of Medicine.14 Navigators are an attractive workforce to support patients engaging with the technology used to capture ePROs, such as symptom monitoring, for patients receiving chemotherapy, particularly, for underserved communities historically supported by navigators.15 Our navigation programs emphasize support for vulnerable populations, including racial and ethnic minority groups (25%), rural residents (30%), and socioeconomically disadvantaged people (10% eligible for Medicare and Medicaid). Our patient navigation workforce is ideally positioned to facilitate the collection of ePROs, as collecting and responding to ePROs aligns with their training and responsibilities. Navigators observe challenges for under-resourced populations when engaging them in technology. Currently, at UAB and MCI, lay and nurse navigators use an electronic medical record (EMR) integrated, web based software – Patient-Reported Outcomes Mobile Platform (PROmPtä) – to capture patient-reported data (symptoms, functional status, depression, and distress) during clinical encounters.16 We are currently implementing a system-wide approach to remote symptom monitoring using this platform (Figure 1). Remote symptom monitoring programs have been associated with improved efficiency of symptom assessment;17-19 patient-clinician communication and satisfaction;20,21 and symptom control and well-being.22-27 In patients with advanced cancer, a randomized trial by Basch and colleagues demonstrated that between visits, weekly electronic home-based, remote symptom monitoring with automated alerts to clinicians (Home ePRO) was associated with reduced emergency department (ED) and hospital visits, improved health-related quality of life, and a 5-month increase in overall survival.28 Importantly, benefits in the remote symptom monitoring randomized control trial were greatest for patients with limited prior computer experience.28 Low digital health literacy may exacerbate disparities. In this era, digital health literacy now should include access to digital technology, use of digital technology to improve health literacy, and using new digital platforms to communicate with the patient’s healthcare team. Digital health literacy is an increasingly important extension of health literacy given the rapid increase in available health technology (e.g., remote symptom monitoring, patient portals).29 Low digital health literacy disproportionately impacts under-resourced patients.30 In a large study of older adults, Black and Latino patients were less likely than White patients to utilize the patient portal. Access to the internet, ability to use the internet, and ability to use email differed by race and ethnicity.29 As such, recommendations for institutions utilizing electronic health technology are available. 31 However, these are not currently leveraged by navigation programs in our region or nationally. Disparities exist in implementation of remote symptom monitoring. We began standard of care implementation of remote symptom monitoring using ePROs in May 2021. Our preliminary data shows that Black patients were less likely to be enrolled (80% vs. 91%) and more likely to withdraw (20% vs. 9%) than White patients. In addition, patients living in rural areas had lower compliance rates (55% vs. 69%) when compared to patients living in urban areas. Supporting this, navigators at MCI and UAB have observed challenges related to both initial engagement of the technology platform and continued use. For example, some patients at the time of enrollment express discomfort with using their smartphone or being confident that 3. Patient completes weekly symptom assessment from home § Patient is notified whenever symptom assessments are due § Patient completes remotely or in the clinic during routine treatments 4. Patient receives weekly education: • Real-time, auto-generated Symptom-Self Management Plan • Delivered directly to patient via preferred method of contact (e.g., text, email) 5. Alert notification of elevated symptom responses sent to message center inbox of RN: • Review longitudinal PRO on dashboard • Determine appropriate clinical Intervention(s) to manage elevated symptom • Documentation of Intervention recorded and sent to EMR via integration • Acknowledgement notification sent to patient 1. Patients diagnosed and discussed treatment with Provider § Provider “Educates & Endorses” the benefits of proactive reporting of symptoms through weekly at-home surveys Remote Symptom Monitoring Model 6. Providers & Pharmacists • Reiterates benefits of PRO • Review PRO and longitudinal trends • Pharmacists may close oral adherence and symptom alerts when speaking with patients 2. Lay Navigator • Enrolls patient in PROmPt® using Carevive’s Self-guided enrollment which does the following: • Educates about benefits of proactive Symptom Monitoring from home • Automates patient registration • Initiates baseline survey • Creates recurring survey schedule based on patient preferences and Nurse’s clinic schedule • Supports contactless enrollment Figure 1: Remote symptom monitoring model: Process and roles of team members they can use technology independently. In addition, patients who have compliance issues after initial sign-up report an assortment of technical issues, including lack of comfort with devices, and in some cases, losing access to cellular service due to unpaid bills. Our navigation teams expressed concerns regarding lack of training to specifically address barriers faced by patients with low digital health literacy. Tools and strategies are available to overcome challenges in technology literacy: As health and technology intersects, tools and interventions are needed to minimize the digital divide and to ensure that healthcare disparities are not exacerbated, such as: 1. Provider-level training in health and digital health literacy. This includes teaching providers on patient centered communication, active listening teach-back, and understanding of social norms, cultural awareness, and the importance of patient/family support. Many health professionals overestimate their understanding of health and technology literacy. Health and technology literate providers can improve knowledge, skills, and intended behaviors related to health and technology literacy. 2. Telemedicine educators. Similar to patient navigators who help cancer patients navigate cancer care, educators focused on technologies such as telehealth have great potential in helping patients use these new technologies. Our institution is currently collaborating with the Cancer Awareness Network (CAN), a community-organized group of cancer survivors who help other patients use technology. This group has successfully piloted a telemedicine educator system for patients, training and equipping them to navigate telemedicine visits on their own independently. 3. Community-based education programs. This includes social marketing campaigns, e-health communication (e.g., apps and websites with health information in plain language), local mass media, advocacy, and social media “influencers.” Assessment of Need: There is a need for training for lay navigators to effectively communicate with and engage patients with low digital health literacy. This project will address this need by (1) evaluating the needs of patients with low digital health literacy, (2) developing a navigation training curriculum on how to best support patients with low digital health literacy, (3) deploying this curriculum across nurse and lay navigators at UAB and MCI, sites that serve high volumes of under-resourced patients, (4) evaluating impact of this curriculum on enrollment and compliance (proportion of survey completed) in home-symptom monitoring of under-resourced populations, (5) refining curriculum and/or deploying other approaches to improving patient engagement based on input from key stakeholders at UAB and MCI, and (5) conducting broad-scale dissemination statewide in partnership with UAB, Mobile Infirmary, Russell Medical Center, MCI and their affiliate sites, the Deep South Cancer Control network, the Alabama Comprehensive Cancer Control Coalition, and our technology partner’s community forum. Target Audience: The target audience for this project will be patients, with a specific focus on: (1) Black patients, (2) patients living in rural areas, and (3) patients living in higher disadvantaged neighborhoods (high Area Deprivation Index scores). The target clinical audience will include lay navigators, nurse navigators, community health workers, and social workers. Project Design and Methods: Setting: UAB and MCI are academic institutions in the state of Alabama serving large African American (~25% at each institution) and rural populations. The education level in Alabama is low, with 15% of residents having high school education or less.32 Alabama has a large number of census block groups with high Area Deprivation Index scores, which reflects the low socioeconomic status of the state (Figure 2). 33 Internet connectivity in Alabama: Currently, 95% of Americans have access to a cell phone and 77% have a smartphone with internet connectivity.34 In May 2019, Alabama passed House Bill 400 which allows electrical providers to use existing and future power networks for high-speed internet in rural communities.35 In recent years, more than $62M in grants were awarded to community partners for the provision of high-speed internet in Alabama communities with limited access.36 Despite these state-level efforts, not all patients will have internet access or a smartphone in the home. For these patients, BCBS-AL has committed philanthropic support to provide smartphones and cellular service for the duration of their active treatment for patients completing home symptom monitoring at UAB and MCI. We are Figure 2. 2015 Area Deprivation Index: State of Alabama. specifically tracking the proportion of patients utilizing each of the following: personal smartphone/computer, another person’s smartphone/computer in home (e.g. spouse), smartphone/computer outside home, or smartphone provided by UAB/MCI with support from BCBS-AL. As part of this initiative, philanthropic dollars are available to provide smartphones with internet to patients who lack technology access. Ongoing projects leveraged for the proposed research: Dr. Rocque is the Principle Investigator and Dr. Young Pierce is a Co-investigator for a National Institute of Nursing Research R01 that is evaluating the implementation of navigator-led implementation of home symptom monitoring at UAB and MCI funded in 2021. Within this project, all patients receiving chemotherapy, immunotherapy, and targeted therapy at the participating institutions are eligible for participation in standard of care home symptom monitoring. As of March 31, we have enrolled 185 patients at UAB and 72 patients at MCI. By the time of study initiation, we will be operational in all cancer subtypes and approach all patients on active therapy. The R01 study includes an in-depth analysis using EMR, data from ePROs, and claims data to capture metrics about implementation, with planned assessment of outcomes for under-resourced populations (Black patients, patients in rural areas, patients with high ADI levels). The data captured within this project provide a foundation for the analysis included in this proposed research. Project Overview: The proposed research will include three phases (Figure 3). In phase I, we will conduct a formative evaluation leveraging our ongoing R01-funded implementation of home symptom monitoring and our network of community health workers understand regional barriers to health technology. We will combine this regional analysis with existing national literature to develop a framework for two tailored educational models targeted for navigators. In Phase II, we will test the educational modules within health systems currently using technology facilitated patient reported outcomes. In Phase III, we will conduct a statewide and national dissemination of the materials developed and refined in Phase I and II of the project. Phase I: Development phase (Months 0-6) Preliminary data analysis: We will conduct a mixed-methods data analysis to inform development of our navigator education. • For the quantitative analysis, we will conduct a preliminary analysis to compare (1) proportions of agreement to participate in home symptom monitoring and (2) discontinuation between Black vs. White patients, rural vs. urban patients, and those living in more vs. less disadvantaged areas. • For the qualitative analysis, we aim to get perspectives from two key stakeholder groups: patients and community health workers. For patients, we will identify 10-20 patients who decline or discontinue participation to assess technology- or communication-related barriers to participation. We will approach these patients at the time that they decline participation or at their subsequent clinic visit after they decline to enhance likelihood of participation. For community health workers, we will invite 10-20 community health workers with expertise in serving communities of interest to elicit perspectives and observations about barriers to technology who have previously worked with collaborator (Hardy). All participants will provide informed consent. Interviews will be conducted either in person, by telephone, or by Zoom based on participant preference. All participants will receive $50 as compensation for their time. Phase I: Development Phase Quantitative analysis: decline and discontinuation of symptom monitoring program Qualitative analysis: community barriers to technology Literature review: barriers to use of health technology Phase II: Testing Phase Training Evaluation: knowledge, barrier awareness, and comfort engaging patients Implementation evaluation: decline and discontinuation of home symptom monitoring post training Phase II: Testing Phase Training Evaluation: knowledge, barrier awareness, and comfort engaging patients Month 0-6 Month 7-18 Month 19-30 Figure 3: Project overview Integration of data with existing literature: We will integrate the data from this preliminary analysis with existing literature on strategies to overcome health and technology literacy challenges, focusing on Black, rural, and populations living in more disadvantaged areas. Develop training curriculum and patient-centric materials: Based on the preliminary data and existing literature, we will develop both a 1-hour training for navigators and other support staff on digital health literacy and strategies to overcome patient-related barriers to using technology (Training Component 1). A second hourlong training will be developed specifically for navigators at UAB and MCI who will be engaging patients in technology-based capture of ePROs (Training Component 2). Finally, we will develop both generic and symptom-monitoring -specific materials that can be leveraged during these encounters and shared with patients to facilitate patient engagement and provide community-based care. Phase II: Testing Phase (Months 7-18) Training: We will conduct in-person training sessions developed in Phase I at UAB, Russell Medical Center (UAB affiliate located in rural Alabama), Mobile Infirmary (UAB partner in Mobile, Alabama), MCI (main and satellite locations in Springhill and Fairhope) with navigators. Evaluation: The evaluation will have two parts, a training evaluation and implementation evaluation: 1. Training evaluation: We will conduct pre- and post-training surveys (administered using REDCap or on paper) at all sites to assess knowledge of health literacy, awareness of potential barriers for patients engaging in technology, and comfort engaging patients with low health literacy or technology barriers. Surveys will be given to those participating on Training Component 1 before and after the in-person or virtual training as to minimize potential of non-completion. We will also capture the number of participants from each organization to demonstrate the reach of the training. 2. Implementation evaluation: This will demonstrate impact of training in digital health literacy (Training Component 1 AND 2). We will evaluate baseline (six months prior to training) and post-training (six months post-training) proportion of patients approach by navigators, patient agreement to participate in home symptom-monitoring, and proportion of patients who miss assessment or stop participation. We will also describe reasons for discontinuation among each patient group. Finally, we will collect semi-structured exit interviews with 10-20 patients from the target patient groups who decline participation or miss surveys. Phase III: Dissemination and Evaluation (Months 18-30): State-wide dissemination: 1. We will conduct our training at the annual Deep South meeting of community health advisors through our partnership with the Office of Community Outreach and Engagement. There is anticipated to be >400 community health advisors in attendance and all will receive the training. 2. In partnership with the Alabama Comprehensive Cancer Control Coalition (ACCC), we will offer a web based version of our training for any care coordinator, lay or nurse navigator, social worker, or other interested staff from other cancer centers and/or health systems across the state of Alabama. This organization brings together clinicians and personnel from cancer centers across the state focused on supportive care, cancer control and cancer prevention. Statewide meetings are conducted quarterly via zoom during the Covid-19 pandemic. This training would fit perfectly with overall mission to increase access to patients for information, new technologies, and improve health disparities in cancer. National dissemination: 1. Through our technology partner, Carevive, we have monthly community forums to help with implementation of ePROs. At present, 32 institutions are engaged with this technology vendor, with locations across the country. We will offer the training to staff from all institutions participating in this collaborative. 2. Dissemination through ACS: We will also video record the training and will provide this for future dissemination. We anticipate that this could be a key module for all future navigator training programs. Evaluation: We will use a similar strategy to evaluate training, as noted in Phase II. We will use a pre-post evaluation to assess knowledge of digital health literacy, awareness of potential barriers for patients engaging in technology, comfort engaging patients with low health literacy or technology barriers, and satisfaction with the training. Pre- and post- surveys will be given to all training participants at immediately before and after training. Analytic Plan: Qualitative components: For each qualitative component, two independent coders will read the transcripts and develop an open coding scheme, which is the process of labeling portions of text to identify all ideas, themes, and issues suggested by the data.37 Analytic codes constructed in the context of open coding are provisional and will be grounded within the data.38 The final version of the coding schema will be reviewed and finalized by the multidisciplinary team, which will include all investigators. The two primary coders will subsequently use NVivo software (QRS International) to conduct “focused coding,” which includes a detailed analysis of themes identified during open coding. Any discrepancies will be resolved by a third coder (GR). Our team has used this approach in prior studies and found it to be a useful strategy in evaluating program implementation.39-41 The process will be repeated until thematic saturation is reached, where no new categories or relevant themes emerge.42 Data from interviews will be analyzed at an aggregate and health system-specific level. Training evaluation: we will use repeated measures models to fit pre-post data on each outcome (i.e., knowledge of health literacy, awareness of potential barriers for patients engaging in technology, and comfort engaging patients with low digital health literacy and/or technology barriers) and estimate average change among navigators. The change estimate will be rescaled as a standardized measure of effect size using the standard deviation at pre-training to aid in interpretation. This analysis is descriptive, and no formal inference will be conducted. Implementation evaluation: For each of the patient proportions of interest (i.e. % enrolled in home symptom monitoring; % missed assessments or withdrew), we will use regression models for binary outcomes with period (pre- vs. post-training implementation) as main explanatory variable, treating the navigators as fixed effects. We will estimate model-adjusted outcome proportions, relative risks, and odds ratios with 95% confidence intervals comparing the between-period estimates. In comparing two groups, at a significance level of 0.05, assuming a reference outcome proportion of 0.6, a sample of 712 (356 per group) provides 80% power to detect a difference in proportions of 0.1 (OR=1.55), i.e., an absolute percentage difference of 10%, which we consider a relevant effect. With a point estimate OR=1.55, this sample size allows for a 95%CI width of 0.98 (i.e., 1.14 – 2.12). Therefore, the expected sample size of >400 patients per time-period will provide adequate precision to proportions and pre-post comparison estimates for UAB and MCI. Qualitative analysis will be conducted using a similar approach to Phase I. Additional reporting for American Cancer Society Navigation Collaboration: A key opportunity for participation in this program is the ability to collaborate to share metrics. UAB and MCI are ideally positioned to participate in this collaboration given not only our long-standing history of navigation, but also our ability to capture data on the program. We anticipate being able to report on all required metrics (Table 1). Operational data is captured in discrete fields within our electronic medical record systems on the navigation caseload. “No show” appointments are identifiable in the EMR. Psychosocial distress and barriers to care are captured within a baseline survey for all new patients that is administered by navigators at UAB and MCI. Treatment compliance, diagnosis to initial treatment, and use of clinical trials are all quality metrics that are captured as part of the quality programs. Dr. Rocque is the Medical Director for Quality in the cancer service line at UAB and Dr. Young Pierce leads the MCI Cancer Control and Prevention program. Thus, this research team is well positioned to capture and report on these metrics. Metric Definition Operations Management Navigation caseload Number of new cancer patients navigated per month No-show rate Number of navigated patients who do not complete a scheduled appointment Psychosocial Support, Assessment Psychosocial support and assessment Number of navigated patients per month who receive psychosocial distress screening at a pivotal medical visit Coordination of Care/Care Transition Barriers to Care Top 3 barriers to care identified by the program Treatment Compliance Percentage of navigated patients who adhere to institutional treatment pathways per quarter Diagnosis to Initial Treatment Average number of days from date of diagnosis to date of first treatment for navigated patients Clinical Trials Education Number of patients educated on clinical trials by the navigators per month Clinical Trials Referral Number of navigated patients per month referred to clinical trials staff Table 1: Metrics reported to the collaborative Deliverables: (1) Summative evaluation of current state of engagement and barriers for under-resourced populations (Phase I); (2) Summative evaluation of training (Phase II and III); (3) Video-recorded training for ACS dissemination; (4) navigation metrics Innovation: This project is innovative for several key reasons: 1. While navigators have traditionally assisted with health literacy and reducing barriers to care, there is very limited former work on using navigators to increase digital health literacy and reduce technology barriers, a key component to make sure that the technology divide does not widen the already existing disparities gap for minorities and rural patients. 2. The proposed initiative leverages an ongoing pragmatic evaluation of navigator-led remote symptom monitoring using ePROs. This infrastructure will enhance feasibility of data capture and integration of training into practice. 3. This proposal focuses on cancer centers with high proportions of under-resourced patients. 4. The novel partnership with a technology company, the state oncology association, and multiple health systems across the state is unique. It has the potential to transition this project into a state-wide initiative to enhance awareness of health technology literacy. Evaluation and Outcomes: The following outcomes will be captured for the project: (1) Education participant: knowledge of health literacy, awareness of potential barriers for patients engaging in technology, and comfort engaging patients with low health literacy or technology barriers (2) Patients: Proportions of patients in target populations who participate in remote symptom monitoring percent, who complete surveys, and who stop participation at UAB and MCI. Anticipated Project Timeline: Phase I (July – December 2022), Phase II (January 2022 – June 2024), Phase III (June 2024 – December 2024) Organization and Partnership Detail: The University of Alabama at Birmingham (UAB) is one of the original NCI-designated cancer centers, now in the 50th year of NCI designation. UAB has an average analytic caseload of 5500 new cases per year. UAB’s patient population includes racial and ethnic minority groups (25%), rural residents (30%), and socioeconomically disadvantaged people (10% eligible for Medicare and Medicaid). Mobile Infirmary Cancer Care (Affiliate site): Infirmary Cancer Care (ICC) is owned by Infirmary Health System, providing care approximately 2000 new cancer patients at three locations in Southwestern Alabama and the Florida panhandle. Medicare/Medicare insured patients comprise approximately 45% of patients treated. 2020 Census reports 13% under the age of 65 are uninsured. Mobile County population demographics: 51% White, 43% Black. UAB Medicine -Russell Medical Cancer Center: Located in Alexander City, Russell Medical Cancer Center (RMC) serves patients in Tallapoosa and the surrounding counties. RMC sees approximately 250 new cancer cases each year; 22% of the population in Tallapoosa County is over the age of 65. Poverty levels in Tallapoosa County is 15%, as reported in the 2020 Census. University of South Alabama Health Mitchel Cancer Institute (MCI): MCI is a member hospital of USA Health, University of South Alabama, and the only academic cancer center in the region. MCI provides care to approximately 3000 new cancer patients at three Mobile and Baldwin Counties locations covering a catchment area of 4 million across 54 counties in Alabama, Mississippi, and Florida including some of the most impoverished counties in the United States. MCI’s patient population includes 25% Black, 55% rural, 14% Medicare, 12% Medicaid, and 2% uninsured patients. Cancer awareness network: Cancer Awareness Network for Children, Inc., (CAN) is a grassroots community organization developed by sisters who wanted to make a difference. They were birth out to the pain of their mother’s lung cancer diagnosis and her early demise over 25 years ago. Their mission is to inform, educate, motivate, and enlighten underserved individuals of all ages who have been diagnosed with cancer. In addition, they provide supportive services and eliminate fears associated with a cancer diagnosis. They also advocate for the health and economic equity of cancer survivors and caregivers and are actively involved in alleviating burdens that many families and survivors of cancer encounter. Their vision is that every cancer patient will receive the medical and integrated help needed to experience quality throughout their lives. Alabama Comprehensive Cancer Control Coalition (ACCCC): ACCCC is the state entity that writes and enacts the state cancer plan through the Alabama Department of Public Health Cancer Control Division. The ACCCC is a group of health care providers, health systems, cancer centers, organizations, cancer patients, and cancer survivors who work to develop and sustain a coordinated, integrated approach to reducing cancer morbidity, and mortality, and improving care for cancer patients and their caregivers. The group meets quarterly to disseminate information and work toward the goals laid out in the state cancer plan. Carevive Systems: Carevive systems was founded in 2013, is an oncology-centered health technology company specializing in patient-reported outcomes, quality-of-life assessment, and treatment and survivorship care plans. The Carevive cloud-based platform enables providers to monitor patient symptoms remotely using electronic patient-reported outcomes and enhance the patient experience and improve patient outcomes. The Carevive platform and its patient-reported outcomes tool, PROmPT™, are integrated into the electronic health records for both UAB and MCI and allow for ready access of health care providers to electronic patient reported outcome data that streams automatically into the patients’ cancer center care record.