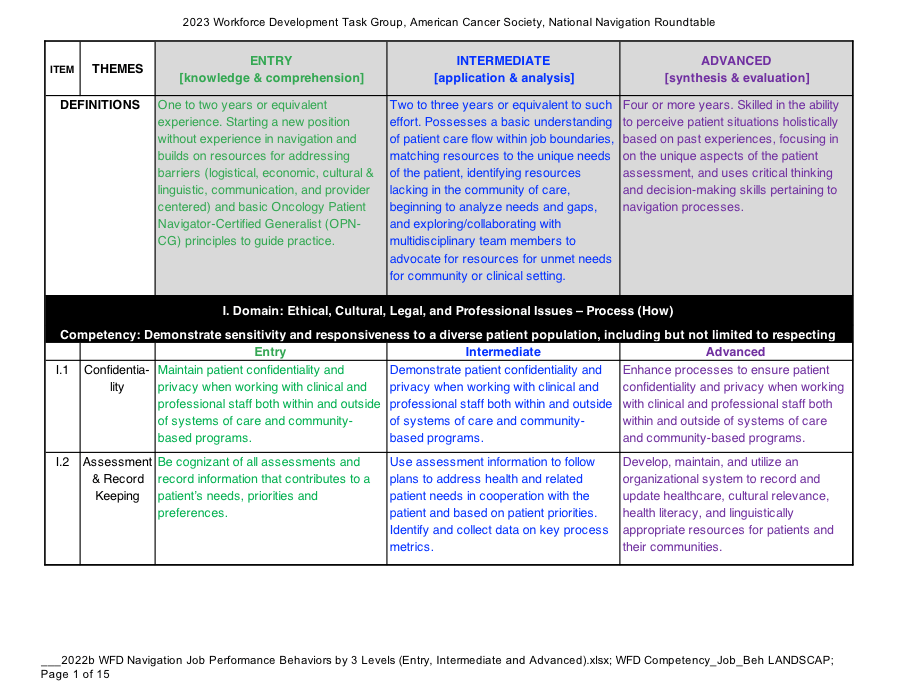
Through the work and consensus of the Workforce Development Task Group, seven training competency domains are recommended by the NNRT for patient navigation.
To build consensus on the domains, the Task Group reviewed well known programs for commonalities, including the Harold P. Freeman Patient Navigation Training Center, the George Washington (GW) University Cancer Center’s Online Academy, the Patient Navigation Training Collaborative, Academy of Oncology Nurse and Patient Navigators, Colorado Public Health and Environment Program’s Patient Navigation Registry Program, and the Oncology Nursing Society.
These domains reflect overlap between programs, with some unique parameters.